Medicare FFS Telehealth Policy During the Federal Government Shutdown (Updated 10/27/25)
Last Updated: October 27, 2025
Beginning October 1, 2025, the expanded Medicare telehealth flexibilities expired as a result of the federal government shutdown. See below for the changes that are currently in effect.
It’s important to note that this policy change applies only to Medicare FFS. Medicare Advantage, Medicaid, and commercial telehealth rules remain unchanged. View the Medicaid Telehealth Policy Manual here.
Background
The expanded Medicare telehealth flexibilities that began during the COVID-19 Public Health Emergency (PHE) expired on October 1, 2025 because of the federal government shutdown. These are the same restrictive rules that were in effect prior to the COVID PHE.
Once the shutdown ends, CMS is expected to reinstate the telehealth flexibilities, but it is unclear whether those flexibilities will be applied retroactively to services delivered on or after October 1.
Health centers can still deliver telehealth during this period, but Medicare FFS will not reimburse most medical telehealth services while the shutdown is active.
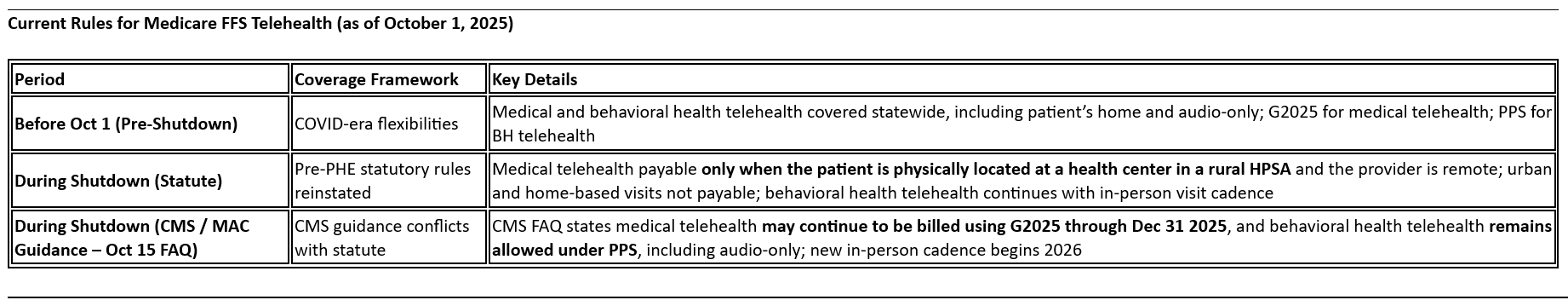
Download PDF of chart here.
FAQ
1. Can health centers still provide telehealth to Medicare FFS patients during the shutdown?
Yes. There is no prohibition on providing telehealth.
Reimbursement depends on whether you follow statutory rules or CMS guidance.
- Under statute: only when the patient is onsite in a rural HPSA and the provider is remote.
- Under CMS FAQ (Oct 15): claims may continue using G2025 through Dec 31, 2025.
Because the FAQ conflicts with statute, CHCANYS recommends proceeding with caution when providing medical telehealth visits to patients with FFS Medicare.
2. Does this apply to Medicare Advantage, Medicaid, or commercial plans?
No. This guidance applies only to Medicare Fee-for-Service.
Medicare Advantage plans, Medicaid, and commercial payers each follow their own telehealth policies, which remain unchanged during the shutdown. View the Medicaid Telehealth Policy Manual here.
3. What counts as a “behavioral health telehealth” service?
Behavioral health telehealth visits continue to be billable under PPS using G0469 (new) or G0470 (established).
These correspond to CPT codes such as 90791, 90792, 90832, 90834, 90837, 90839, and 90845.
If a provider bills an E/M code (e.g., 99213 for medication management), it rolls up to G0467 (medical telehealth) and follows the medical telehealth rules above.
For official CMS guidance, click here
4. What are the rules for the in-person visit requirement for behavioral health?
The new in-person cadence begins January 1, 2026.
- New patients: an in-person visit with the same provider or a member of the same clinical team within six months prior to the first tele-behavioral health visit.
- Established patients: an in-person visit with the same provider or a member of the same clinical team within twelve months.
This applies to all behavioral health telehealth services, including those provided by psychiatrists using E/M codes.
5. What are the rules for audio-only behavioral health?
Audio-only telehealth for behavioral health is still permitted when video is not available or not feasible for the patient, as long as the service otherwise meets Medicare telehealth requirements. This applies in both rural and urban settings.
6. Where can I read more official guidance?
- CMS Telehealth Coverage Overview
- 10-1 Update: Telehealth FAQ CY 2025
- CMS Telehealth Updates Email
- CMS Guidance on G-Codes for FQHCs
Key Takeaways
- Applies to Medicare FFS only.
- Statute: medical telehealth payable only when patient is onsite in rural HPSA and provider is remote.
- CMS FAQ: allows billing G2025 through Dec 31 2025; BH telehealth under PPS remains allowed.
- In-person requirement (BH only): 6 months (new), 12 months (established) starting 2026.
- CHCANYS guidance: CMS and MACs say claims can be submitted, but use caution until shutdown ends.
